Tips for Success: NY Medicaid EHR Incentive Program
June 27, 20192018 Million Hearts® Hypertension Control Champions
June 27, 2019Crown Medical: Transforming Clinical Practice

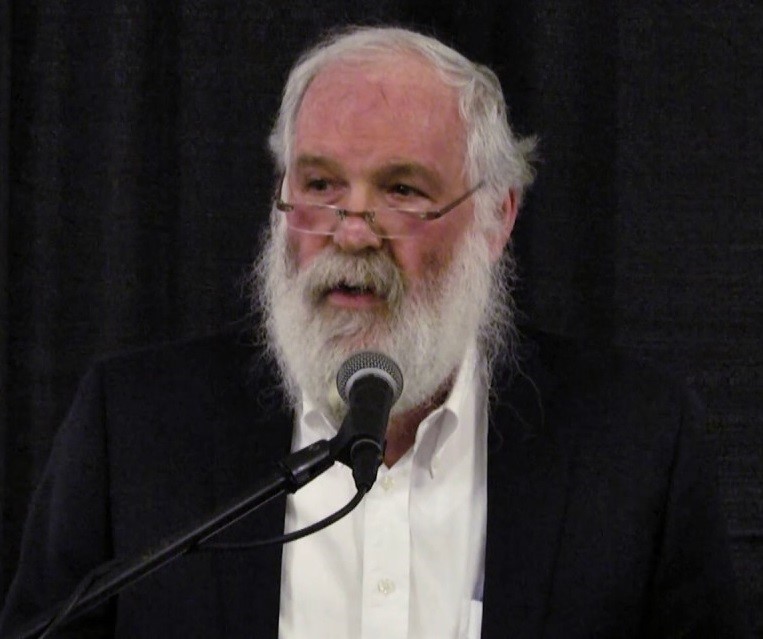
Dr. Eli Rosen, co-founder of Crown Medical
Crown Medical is an adult internal medicine practice in Crown Heights, Brooklyn. The practice has three doctors, two physician assistants, two registered dieticians, and two registered nurses. Most of the practices’ patients (about 9,000 seen per year) are on Medicaid and are members of the Chabad-Lubavitch community.
Crown Medical has been recognized as an “exemplary” practice by the New York State Practice Transformation Network for its success in the Transforming Clinical Practice Initiative (TCPI). Although the initiative is coming to a close this year, Crown Medical continues participation in other quality improvement programs with shared goals. We review below how Crown Medical has transformed patient care through these programs, with support from NYC REACH.
Value-Based Payment
The key goal of TCPI was to prepare providers for value-based payment (VBP) arrangements, in which providers are incentivized to lower patient costs. Through TCPI, Crown Medical developed a new approach to patient cost evaluation. The practice found that patients were accessing far more ancillary services (lab testing, imaging, medical equipment) than the national average. They also noticed high patient costs in evaluation and management services charged to other providers, which led the practice to focus more on care coordination. The practice now thinks beyond the costs of seeing patients in office to the costs of patients using a number of different services. Cost assessment and reduction is now part of the practices’ VBP strategy.
Another way the practice keeps total cost of care down is through out of office care. Home visits have always been a part of the practice’s culture. In case of an emergency, the practice has a volunteer ambulance service bring patients directly to the practice or chief physician’s home before using emergency department services.
Medical Home Operations
The practice aims to be a patient-centered medical home in every sense of the term; putting patients first in every clinical and business decision. Dr. Eli Rosen, the practice’s founder, feels it is his mission in life to be a “village doctor,” a reliable source of care for the whole neighborhood.
The practice maintains New York State Patient-Centered Medical Home (NYS PCMH) Recognition, and has found that participating in the program helped to improve quality metrics and prepare the practice for success in the value-based payment landscape. The practice is able to hire staff to perform care coordination activities by consistently implementing NYS PCMH principles and meeting Healthcare Effectiveness Data and Information Set (HEDIS) measures.
New Revenue Streams
Crown operates a robust Medicare Chronic Care Management (MCCM) program, which allows the practice to provide extensive reimbursed care coordination services to older patients with multiple chronic conditions. The practice supports about 300 elderly patients per month, monitoring their chronic conditions and coordinating care with numerous specialists.
Quality Improvement
The practice designs Quality Improvement projects to meet Merit-Based Incentive Payment System measures and other program goals. Through the HealthyHearts NYC program, for example, the practice started using a new tobacco screening form and raised its screening rate from 80% to 97% in one year.
The practice is currently piloting a new patient activation measurement (PAM) tool with chronic care management patients. This tool helps practice staff assess a patient’s level of engagement and health literacy. Providers can design targeted interventions based on this assessment and use the tool to track improvements in patient activation in a structured format.
Keys to Success
The practice credits its success with two things. First, a mission-driven, patient-centric culture, and second, a willingness to try new programs and tools. Their advice to other practices? Be open to new programs. Find out what government programs may be offered in your area, and seek out new revenue streams.
